Update: Jeremy has now written an article about masks in The Conversation lengthy FAQ. Trisha and Jeremy are two of over hundred of the world’s top academics who released an open letter to all U.S. governors asking that “officials require cloth masks to be worn in all public places, such as stores, transportation systems, and public buildings.”
Confused about mask wearing? Sure, it’s complicated. But not as complicated as some people imply. We’ve been looking at the science (see our papers Face Masks Against COVID-19: An Evidence Review — with 104 references! — and Masks for the public: laying straw men to rest). Here’s a summary of the different streams of evidence, and our take on what it all means.
Translations
We’d love your help translating this article! Please at-mention @jeremyphoward on Twitter with your translation, and I’ll retweet it and add it here.
- Italian (published in the journal Evidence)
- Spanish (from @tyoc213)
- German (from André Calero Valdez)
- French (from GitHub user Bnech)
- Greek (from @a8inea)
- Swedish (from Christoffer Björkskog)
- Dutch (from David Smeijer)
- Finnish (from Thomas Brand)
- Portuguese (from Leandro Gomide); also see earlier PDF translation from @CeliaDeus1
- Romanian (from Emilian Bold)
- Turkish (from Zikri Bayraktar)
- Estonian (from Kaur Maran)
- Hungarian (from Ago Lajko)
- Chinese (Simplified) (from @HFProjectOrg)
- Chinese (Traditional) (from @HFProjectOrg)
- Japanese (from perapera.ai)
- Indonesian (from Lailaturrahmi)
- Hindi (from GitHub user alephthoughts)
- Nepalese (from Vidya Sagar Gurung)
- Hebrew (from Motti Haimi)
- Arabic (from Ali Alsahlanee)
The epidemiology of disease spread
You’ve probably seen the videos of closely-packed dominos and mousetraps, where a single item fires off a huge cascade. The closer the dominos (or mousetraps), the more chaos gets generated. Every infectious disease has a transmission rate (R0). A disease with an R0 of 1.0 means that every infected person, on average, infects one other person. A disease whose R0 is less than 1.0 will die out. The strain of flu that caused the 1918 pandemic had an R0 of 1.8. The R0 of the virus which causes COVID-19 was estimated at 2.4 by Imperial College researchers, although some research suggests it could be as high as 5.7. This means that without containment measures, COVID-19 will spread far and fast. Importantly, COVID-19 patients are most infectious in the early days of the disease (To et al. 2020; Zou et al. 2020; Bai et al. 2020; Zhang et al. 2020; Doremalen et al. 2020; Wei 2020), during which they generally have few or no symptoms.
The physics of droplets and aerosols
When you speak, tiny micro droplets are ejected from your mouth. If you’re infectious, these contain virus particles. Only the very largest droplets end up surviving more than 0.1 s before drying out and turning into droplet nuclei (Wells 1934; Duguid 1946; Morawska et al. 2009) that are 3-5 times smaller than the original droplet itself, but still contain some virus.
That means that it’s much easier to block droplets just as they come out of your mouth, when they’re much larger, compared to blocking them as they approach the face of a non-infected person who is on the receiving end of those droplets. But this isn’t what most researchers have been looking at…
The material science of masks
Debates about the effectiveness of masks often assume that the purpose of the mask is to protect the wearer, since this is what all doctors learn about in medical school. Cloth masks are relatively poor (though not entirely ineffective) at this. For 100% protection, the wearer needs a properly fitted medical respirator (such as an N95). But cloth masks, worn by an infected person are highly effective at protecting the people around them. This is known as “source control”. And it is source control that matters in the debate about whether the public should wear masks.
If you have COVID-19 and cough on someone from 8 inches away, wearing a cotton mask will reduce the amount of virus you transmit to that person by over 90%, and is even more effective than a surgical mask. The researchers who did this experiment described the reduction as “ineffective”, partially based on an inappropriate analysis in which the patients where the cotton masks were perfectly effective were deleted. We disagree with their conclusion. It means you’ll transmit less than 1/10th of the amount of virus you would otherwise have done, decreasing the viral load, which is likely to lead to a lower probability of infection, and fewer symptoms if infected.
The mathematics of transmission
Mathematical modeling by our team, supported by other research (Yan et al. 2019), suggests that if most people wear a mask in public, the transmission rate (“effective R”) can go beneath 1.0, entirely stopping the spread of the disease. The mask doesn’t have to block every single viral particle, but the more particles it blocks, the lower the effective R.
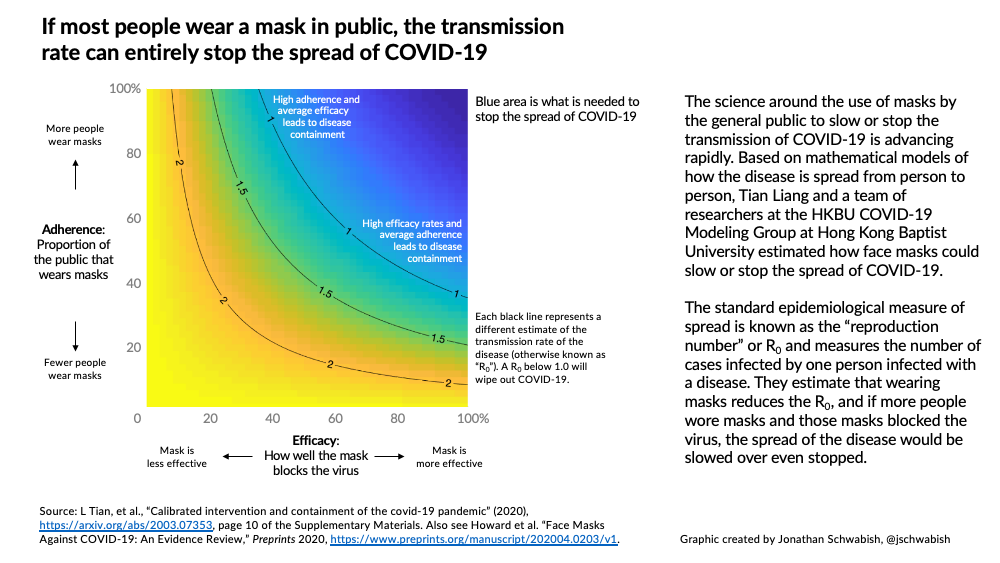
Just how effective mask-wearing is depends on three things illustrated in the diagram: how well the mask blocks the virus (‘efficacy’: horizontal axis), what proportion of the public wear masks (‘adherence’: vertical axis), and the transmission rate of the disease (R0: the black lines on the graph). The blue area of the graph indicates an R0 below 1.0, which is what we need to achieve to wipe out the disease. If the mask blocks 100% of particles (the far right of the graph), even low adherence rates will lead to containment of the disease. Even if masks block a much lower proportion of viral particles, the disease could still be contained – but only if most or all people wear masks.
The political science of mask-wearing
How do you get all or most people to wear masks? Well, you can educate them and try to persuade them, but a more effective approach is to require them to wear a mask, either in specific settings such as public transportation or grocery stores or even at all times outside the home. Research on vaccination (Bradford and Mandich 2015) shows that jurisdictions which set a higher bar for vaccine exemptions have higher vaccination rates. The same approach is now being used to increase mask wearing compliance, and early results (Leffler et al. 2020) suggest that these laws are effective at increasing compliance and slowing or stopping the spread of COVID-19.
Mask-wearing experiments: artificial and natural
An artificial experiment is when a researcher allocates people (usually at random – hence the term ‘randomized controlled trial’ or RCT) to either wearing a mask or not wearing a mask (the control group). There have been no RCTs of mask-wearing by members of the public in COVID-19. RCTs of mask-wearing to prevent other diseases (such as influenza or tuberculosis) have tended to show a small effect which in many studies was not statistically significant. In most such studies, people assigned to the mask-wearing group didn’t always wear their masks.
A natural experiment is when we study something that is really happening – for example when a country introduces a policy of wearing masks. South Korea, for example, had rapid community spread that tracked the trajectory in Italy in the initial weeks. Then, in late February 2020, the government provided a regular supply of masks to every citizen. From that point, everything changed. As Italy’s death count accelerated to horrific levels, South Korea’s actually started decreasing. Here’s South Korea’s number of reported cases (red), and Italy’s (blue); take a close look at what happened in early March, as the impact of the mask distribution kicked in (this South Korean analysis is thanks to Hyokon Zhiang and visualization by Reshama Shaikh:
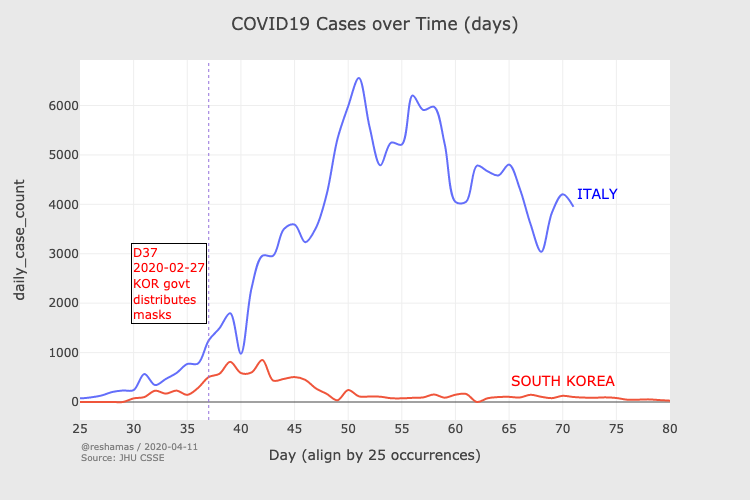
Natural experiments are scientifically imperfect, because there is no direct control group so we can’t be sure that any change is due to the masks. In some countries that introduced mask-wearing, other measures such as strict social distancing, school closures, and cancellation of public events happened at around the same time. Even in these cases, we can find relevant comparisons. For instance, European neighbors Austria and Czechia introduced social distancing requirements on the same date, but Czechia also introduced mandatory mask wearing. The Austrian case rate continued its upward trajectory, whilst Czechia’s flattened out. It wasn’t until Austria also introduced mask laws weeks later that the two counties returned to similar trajectories.
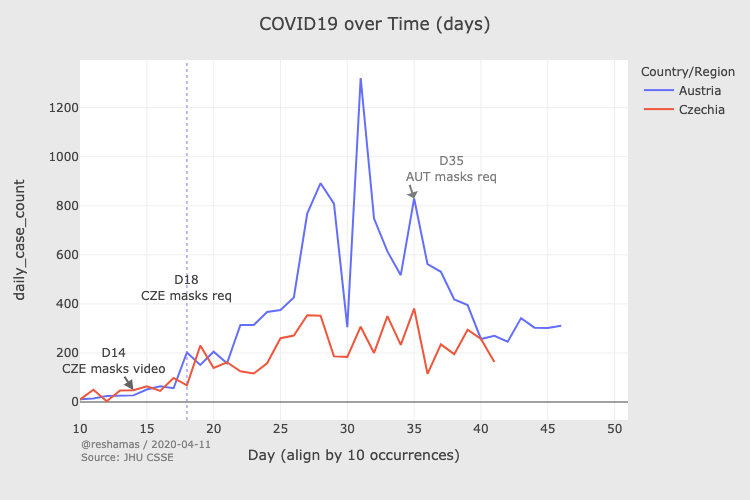
Importantly, in every country and every time period where mask usage has been encouraged through laws, or where masks were provided to citizens, case and death rates have fallen.
The behavioral science of mask wearing
Some have claimed that making (or strongly encouraging) people to wear masks will encourage risky behavior (Brosseau et al. 2020) (for example, going out more, washing hands less), with a net negative result, and this effect was seen in some experimental trials of masks. Similar arguments have previously been made for HIV prevention strategies (Cassell et al. 2006; Rojas Castro, Delabre, and Molina 2019) and motorcycle helmet laws (Ouellet 2011). However, real-world research on these topics found that even though some individuals responded with risky behavior, at a population level there was an overall improvement in safety and well-being (Peng et al. 2017; Houston and Richardson 2007).
The economics of mask-wearing
Economic analyses consider how much it costs to provide masks with how much value (both financial and non-financial) might be created – and, potentially, lost – if they are provided. Such economic studies (Abaluck et al. 2020) indicate that each mask worn by one person (which costs almost nothing) could generate economic benefits of thousands of dollars and save many lives.
The anthropology of mask-wearing
Mask-wearing by the public has been normalized in many Asian countries, partly for individual reasons (to protect against pollution) and partly for collective ones (as a result of recent MERS and SARS epidemics). My mask protects you; yours protects me. However, in most of these countries the norm has been to only wear a mask if you have symptoms; it’s only in recent weeks, as awareness of asymptomatic spread has become better understood, that mask wearing regardless of symptoms has become common.
Conclusion
Whilst not every piece of scientific evidence supports mask-wearing, most of it points in the same direction. Our assessment of this evidence leads us to a clear conclusion: keep your droplets to yourself – wear a mask.
You can make one at home, from a t-shirt, handkerchief, or paper towel, or even just wrap a scarf or bandana around your face. Ideally, use tightly woven fabric that you can still breathe through. Researchers recommend including a layer of paper towel as a disposable filter; you can simply slide it between two layers of cloth. There is no evidence that your mask needs to be made with any particular expertise or care to be effective for source control. You can put a cloth mask in the laundry and reuse it, just like you re-use a t-shirt.
If it turns out that you’re incubating COVID-19, the people you care about will be glad you wore a mask.
Epilogue: Jeremy’s Illustration of Source Control
Here’s a little illustration of source control from Jeremy!
References
- Abaluck, Jason, Judith A. Chevalier, Nicholas A. Christakis, Howard Paul Forman, Edward H. Kaplan, Albert Ko, and Sten H. Vermund. 2020. “The Case for Universal Cloth Mask Adoption and Policies to Increase Supply of Medical Masks for Health Workers.” SSRN Scholarly Paper ID 3567438. Rochester, NY: Social Science Research Network. https://papers.ssrn.com/abstract=3567438.
- Bai, Yan, Lingsheng Yao, Tao Wei, Fei Tian, Dong-Yan Jin, Lijuan Chen, and Meiyun Wang. 2020. “Presumed Asymptomatic Carrier Transmission of Covid-19.” Jama.
- Bradford, W David, and Anne Mandich. 2015. “Some State Vaccination Laws Contribute to Greater Exemption Rates and Disease Outbreaks in the United States.” Health Affairs 34 (8): 1383–90.
- Brosseau, Lisa M., ScD, Margaret Sietsema, PhD Apr 01, and 2020. 2020. “COMMENTARY: Masks-for-All for COVID-19 Not Based on Sound Data.” CIDRAP. https://www.cidrap.umn.edu/news-perspective/2020/04/commentary-masks-all-covid-19-not-based-sound-data.
- Cassell, Michael M, Daniel T Halperin, James D Shelton, and David Stanton. 2006. “Risk Compensation: The Achilles’ Heel of Innovations in Hiv Prevention?” Bmj 332 (7541): 605–7.
- Doremalen, Neeltje van, Trenton Bushmaker, Dylan H. Morris, Myndi G. Holbrook, Amandine Gamble, Brandi N. Williamson, Azaibi Tamin, et al. 2020. “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1.” New England Journal of Medicine 0 (0): null. https://doi.org/10.1056/NEJMc2004973.
- Duguid, JP. 1946. “The Size and the Duration of Air-Carriage of Respiratory Droplets and Droplet-Nuclei.” Epidemiology & Infection 44 (6): 471–79.
- Houston, David J, and Lilliard E Richardson. 2007. “Risk Compensation or Risk Reduction? Seatbelts, State Laws, and Traffic Fatalities.” Social Science Quarterly 88 (4): 913–36.
- Leffler, Christopher, Edsel Ing, Craig A. McKeown, Dennis Pratt, and Andrzej Grzybowski. 2020. “Country-Wide Mortality from the Novel Coronavirus (COVID-19) Pandemic and Notes Regarding Mask Usage by the Public.”
- Morawska, LJGR, GR Johnson, ZD Ristovski, Megan Hargreaves, K Mengersen, Steve Corbett, Christopher Yu Hang Chao, Yuguo Li, and David Katoshevski. 2009. “Size Distribution and Sites of Origin of Droplets Expelled from the Human Respiratory Tract During Expiratory Activities.” Journal of Aerosol Science 40 (3): 256–69.
- Ouellet, James V. 2011. “Helmet Use and Risk Compensation in Motorcycle Accidents.” Traffic Injury Prevention 12 (1): 71–81.
- Peng, Yinan, Namita Vaidya, Ramona Finnie, Jeffrey Reynolds, Cristian Dumitru, Gibril Njie, Randy Elder, et al. 2017. “Universal Motorcycle Helmet Laws to Reduce Injuries: A Community Guide Systematic Review.” American Journal of Preventive Medicine 52 (6): 820–32.
- Rojas Castro, Daniela, Rosemary M Delabre, and Jean-Michel Molina. 2019. “Give Prep a Chance: Moving on from the ‘Risk Compensation’ Concept.” Journal of the International AIDS Society 22: e25351.
- To, Kelvin Kai-Wang, Owen Tak-Yin Tsang, Wai-Shing Leung, Anthony Raymond Tam, Tak-Chiu Wu, David Christopher Lung, Cyril Chik-Yan Yip, et al. 2020. “Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study.” Lancet Infect. Dis. 0 (0). https://doi.org/10.1016/S1473-3099(20)30196-1.
- Wei, Wycliffe E. 2020. “Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020.” MMWR. Morbidity and Mortality Weekly Report 69. https://doi.org/10.15585/mmwr.mm6914e1.
- Wells, WF. 1934. “On Air-Borne Infection: Study Ii. Droplets and Droplet Nuclei.” American Journal of Epidemiology 20 (3): 611–18.
- Yan, Jing, Suvajyoti Guha, Prasanna Hariharan, and Matthew Myers. 2019. “Modeling the Effectiveness of Respiratory Protective Devices in Reducing Influenza Outbreak.” Risk Analysis 39 (3): 647–61. https://doi.org/10.1111/risa.13181.
- Zhang, Juanjuan, Maria Litvinova, Wei Wang, Yan Wang, Xiaowei Deng, Xinghui Chen, Mei Li, et al. 2020. “Evolving Epidemiology and Transmission Dynamics of Coronavirus Disease 2019 Outside Hubei Province, China: A Descriptive and Modelling Study.” The Lancet Infectious Diseases 0 (0). https://doi.org/10.1016/S1473-3099(20)30230-9.
- Zou, Lirong, Feng Ruan, Mingxing Huang, Lijun Liang, Huitao Huang, Zhongsi Hong, Jianxiang Yu, et al. 2020. “SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients.” New England Journal of Medicine 382 (12): 1177–9. https://doi.org/10.1056/NEJMc2001737.