Summary: SARS-CoV-2 particles do not float freely in the air. They are expelled as relatively large droplets, which research shows are easily caught by a simple cloth or paper mask. If an infected person doesn’t wear a mask, their droplets quickly evaporate into smaller droplet nuclei, which are harder to filter with a cloth mask. However there are some cloth mask designs which can do a very good job of this too.
I’ve seen a lot of confusion about the efficacy of mask filtration, and the impact of masks on re-breathing CO2. In each case, part of the problem is based on a failure to understand the relevant particles, and particle sizes. So let’s see if we can resolve some of the confusion!
Here are some basic parameters (all approximate measurements):
- The SARS-CoV-2 virus particle is 100nm (nanometers) in diameter.
- A CO2 molecule is 0.33nm diameter.
- When we speak we produce droplets between 20 and 2000µm (micrometers) in diameter. Note that a micrometer is a thousand times larger than a nanometer!
- Larger droplets fall to the ground fairly quickly. Smaller droplets evaporate in (at most) a few seconds to a droplet nuclei of around 1µm.
- A 27µm droplet would carry 1 virion on average, and would evaporate to 5µm in a few seconds.
- Small particles do not fly straight through materials, but instead follow brownian motion, resulting in them coming in contact with a material even when the material weave is larger than the particle.
- Many materials, such as paper towel, have a complex weave which make it very difficult for particles to fully penetrate.
- Materials like chiffon and silk also have electrostatic effects that result in charge transfer with nanoscale aerosol particles, making them particularly effective (considering their sheerness) at excluding particles in the nanoscale regime (<∼100 nm).
So, the first thing to note is that CO2 is going to flow through any mask without any trouble. There is no known mask material that will filter 0.33nm molecules. If it did, you wouldn’t be able to breathe at all!
The size of the virus particle itself is not relevant to any discussion of mask filtration. This is because virus particles never float freely in the air, but are always at least suspended in a droplet nuclei ten times larger than the virus itself. A droplet containing a single particle will on average start out 270 times larger than the virion, and will evaporate to nuclei of 50 times larger than the virion.
The size of the weave of the fabric is also not directly comparable to the size of the droplets or droplet nuclei, due to the three dimensional nature of many types of material, the indirect route taken by small particles in brownian motion, and the electrostatic effects in many materials. So if you’ve seen those claims that masks can’t possibly stop COVID-19 because the virus is too small, now you know why they’re totally wrong.

Therefore, the only way to really understand the efficacy of a mask is to actually test it in practice. Because the size of droplets that are ejected are much larger than those that remain in the air (due to evaporation), testing must be done separately for source control (protecting others from the wearer) vs PPE (protecting the wearer from others).
Source control efficacy
There are two main ways to physically test a mask:
- Have someone wearing it breathe, talk, cough, and so forth, or
- Synthetically simulate these actions using a spray mechanism, such as a nebulizer.
Because actual human actions are complex and hard to simulate correctly, the first approach is preferred where possible. Generally, we are most interested in speech droplets, because people that are coughing and sneezing should stay home, so those are of less importance to community transmission, and breathing is not believed to contain significant concentrations of SARS-CoV-2 particles.
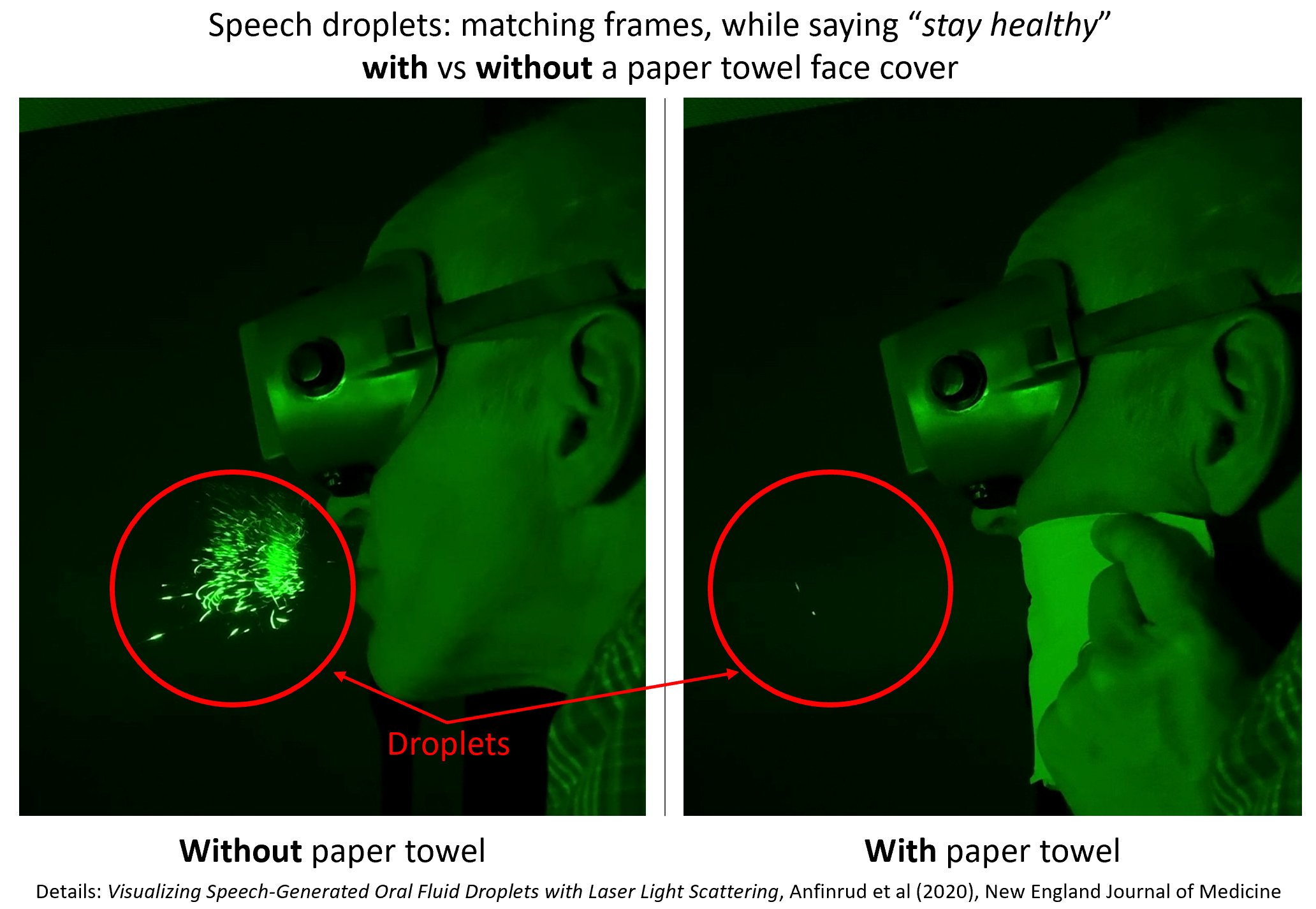
There is a study that looked at the protective effect of a simple cloth mask for speech droplet source control, that found that approximately 99% of the forward-facing droplets visible in a laser chamber were blocked. The cloth mask in the study was moist, in order to avoid dust contamination of the equipment; a followup experiment from the same group, pictured here (but not published yet), found that a dry paper towel had the same results.
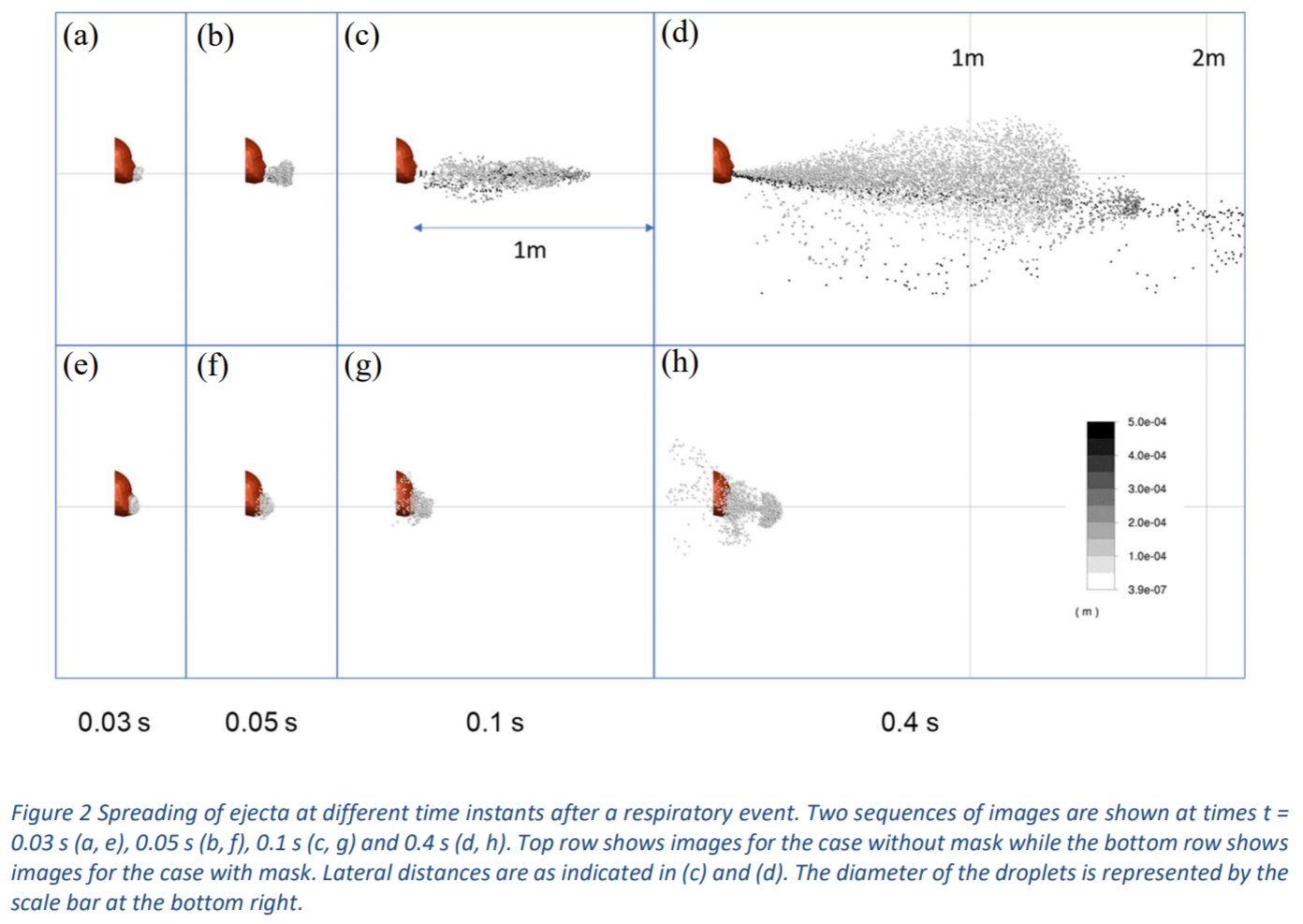
There are no studies that have directly measured the filtration of smaller or lateral particles in this setting, although using Schlieren imaging it has been shown that all kinds of masks greatly limit the spread of the droplet cloud, consistent with a fluid dynamic simulation that estimated this filtration level at 90%.
Another approach to studying source control efficacy tested viral shedding in respiratory droplet samples and aerosol samples. In this study, seasonal coronavirus was tested, which is in the same genus as SARS-CoV-2. Cloth masks were not tested; neither were speech droplets – only breathing and coughing were studied. An unfitted surgical mask was 100% effective at blocking coronavirus particles.
In a pair of studies from 50 years ago, a portable isolation box, provided with a filtered air supply and a means of access for a test subject’s head, was attached to an Andersen Sampler and used to measure orally expelled bacterial contaminants before and after masking. In one of the studies, during talking, unmasked subjects expelled more than 5,000 bacterial contaminants per 5 cubic feet; 7.2% of the contaminants were associated with particles less than 4μm in diameter. Masked subjects (using a cotton muslin and flannel blend) expelled an average of 19 contaminants per 5 cubic feet; 63% were less than 4μm in diameter. So overall, over 99% of contaminants were filtered. The second study used the same experimental setup, but studied a wider range of mask designs, including a 4-ply cotton mask. For each mask design, over 97% contaminant filtration was observed.
PPE efficacy
Protection of the wearer (PPE) is much more challenging that source control, since, as discussed, the particles are much smaller (although not as small as a free virion). It’s also much harder to directly test mask efficacy for PPE using a human subject, so instead simulations must be used. There are two considerations when looking at efficacy:
- The filtration of the material
- The fit of the design.
There are many standards around the world for both of these issues, such as the U.S. National Institute for Occupational Safety and Health (NIOSH) N95 classification. The ‘N95’ designation means that when subjected to careful testing, the respirator blocks at least 95 percent of very small (0.3 micron) test particles. These are much smaller than virus-carrying droplets or droplet nuclei, which means that masks that do not meet this standard may be effective as PPE in the community.
One recent study looked at the aerosol filtration efficiency of common fabrics used in respiratory cloth masks, finding that efficacy varied widely, from 12% to 99.9%. Underlining the importance of fit for specialized medical masks, an unfitted N95 respirator had the worst efficacy. Many materials had >=96% filtration efficacy for particles >0.3 microns, including 600 TPI cotton, cotton quilt, and cotton layered with chiffon, silk, or flannel. These findings support studies reported in 1924 by Wu Lien Teh, which described that a silk face covering with flannel added over the mouth and nose was highly effective against pneumonic plague.
Many studies use very small aerosol particles at very high flow rates, such as a study that was used as the basis for a table in WHO’s Advice on the use of masks in the context of COVID-19. In this study, tiny 78nm aerosol particles were blasted through cloth at a rate of 95 liters per minute. Only N95 and equivalent masks were able to stand up to this torrent of aerosol, which would never be seen in practice in any normal community setting. The machines used for these studies are specifically designed for looking at masks that hold their shape (respirators) which are glued or attached with beeswax firmly to the testing plate. Flexible masks such as cloth and surgical masks can get pulled into the hole in the testing plate.
There are many designs of cloth masks, with widely varying levels of fit. There have been few tests of different designs. One study looked at unfitted surgical masks, and used three rubber bands and a paper clip to improve their fit. All eleven subjects in the test passed the N95 fit test using this approach. A simple mask cut from a t shirt achieved a fit score of 67, not up to the 100 level required for N95, but this mask offered substantial protection from the challenge aerosol and showed good fit with minimal leakage. Wu Lien Teh noted that a rubber support could provide good fit, although he recommended that a silk covering for the whole head (and flannel sewed over nose and mouth areas), with holes for the eyes, tucked into the shirt, is a more comfortable approach that can provide good protection for a whole day.
Overall, it appears that cloth face covers can provide good fit and filtration for PPE, but results will vary a lot depending on material and design.
Conclusion
Overall, there is evidence that simple cloth face masks will generally provide good protection to those around the wearer (source control). This is possible because droplets expelled during speech are much larger than the droplet nuclei they later turn into through evaporation.
There are also some combinations of material and design which can provide good protection to the wearer as well (PPE). However, many cloth masks do not have the materials or design necessary to achieve the highest level of protection.